Skin Cancer Care -A Massive health Risk in Australia
Article Research and Experiential investigation by Axel Ritenis & Editing,Fact Checking & References by Lauren Richardson
– Australia’s Skin Cancer Crisis – A Silent Epidemic Demanding Urgent Action
-Alarming Statistics and the Grim Reality
Skin cancer is a major cause of illness in Australia. We have the world’s highest skin cancer rates, with two out of three Australians developing this disease in their lifetime. Melanoma, the deadliest form, claims thousands of lives annually, casting a long shadow over the sun-drenched nation.
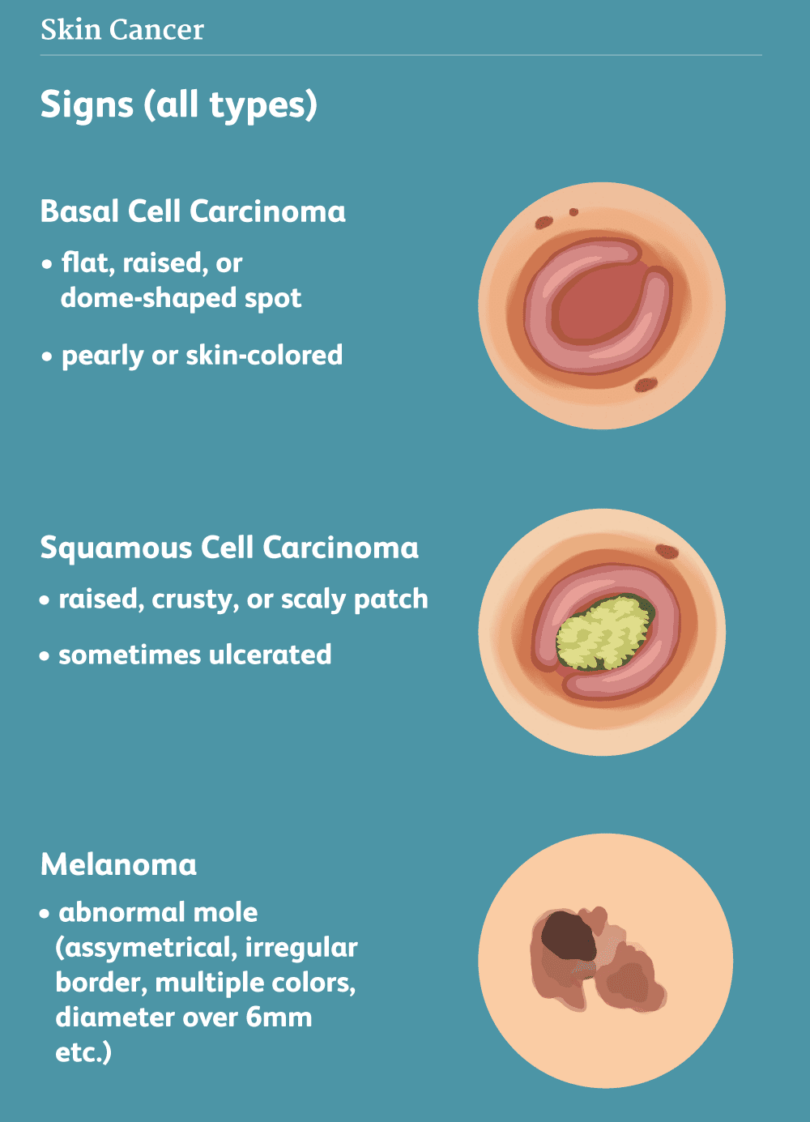
The two most common types of skin cancers are basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), collectively called keratinocyte carcinoma (KC).
The skin is the largest organ in the human body. Its main functions include protecting the inner layers and organs from external elements, regulating body temperature and preventing dehydration.
The three main types of skin cells in the human body are:
- basal cells, which make up the lower layer of the skin
- squamous cells, which make up the top layer of skin
- melanocytes, which produce dark pigment that gives colour to the skin (melanin).

Rising rates of hospitalisation for skin cancer, and the strain it has on the healthcare system has prompted the Melanoma Institute Australia to call for free melanoma screening for high-risk Australians, which may include people with red hair, lots of moles or a history of skin cancer. The institute’s cancer epidemiologist Professor Anne Cust said a screening program would ensure people at high risk can access high-quality skin checks at an appropriate time for free.
Although less common, melanoma has much higher mortality than KC. Australia and New Zealand have the highest incidence of melanoma and KC in the world. High ambient ultraviolet radiation exposure and a large number of fair-skinned residents of European origin are significant contributing factors of this. Exposure to ultraviolet radiation accounts for almost all KC’s and over 80 per cent of melanoma. Collectively, nearly 20,000 new cases of malignant melanoma are diagnosed in Australia and New Zealand annually.
Analysing Health Care Costs related to Skin cancer
The financial burden of skin cancer treatment in Australia is staggering, costing the healthcare system over $1 billion annually and continuing to rise.
The incidence of KC is over 30 times higher than melanoma. The high incidence of skin cancers, and the resources used in their management, translates to a high cost burden. In Australia, the approximate first-year costs of melanoma per patient ranged from AU$644 for melanoma in situ to AU$100,725 for unresectable stage III/IV disease.
For patients with more advanced stages of melanoma, new high-cost systemic pharmacotherapies have been approved for Government subsidy, as a part of Australia and New Zealand’s universal healthcare systems.
Australian-wide direct costs to the Government for newly diagnosed patients with melanoma were AU$397.9 m and AU$426.2 m for KCs, a total of AU$824.0 m.
Researchers have found that skin cancer-related conditions accounted for three percent of all problems managed in general practice. Exposure to ultraviolet radiation can be prevented, meaning a large proportion of skin cancers can also be prevented through sun protection measures.
Cancer Council Australia considers the “Slip Slop Slap” campaign, launched in 1981, to be “one of the most successful health campaigns in Australia’s history”. It focused on preventative actions to decrease the likelihood of skin cancer, and highlighted the potential cost-savings to the Government of public health skin cancer prevention programs and policies.
Despite some reports that melanoma incidence in younger adults is declining, healthcare costs of skin cancer are expected to rise further due to the joint effects of health price inflation, new technologies and medicines, and ageing demographics. Skin cancer prevention campaigns require financial commitment by Governments and interest groups. Currently, the dermatology workforce in both Australia and New Zealand is under significant pressure to manage the vast numbers of new and existing patients with skin cancers. Given that skin cancer prevention campaigns are effective and cost-effective in both the short and long term , it is critical that greater investment in prevention occurs to ensure more sustainable and efficient health systems.
The Cost Barrier: A Matter of Life and Death
A study on the estimated healthcare costs of skin cancers in Australia and Aotearoa New Zealand conducted in 2021 showed hospitalisations for skin cancer are on the rise.
In 2023, Cancer Australia estimated over 18 thousand new cases of skin cancer would be diagnosed. Of this, they estimated over 1’300 people would die. Cancer Australia said a person has an almost 6 per cent chance of receiving a diagnosis by the age of 85.
The survival rate of melanoma of the skin is relatively high. Between 2015 and 2019, 94 percent of people diagnosed were still alive five years later.
Despite this and Medicare’s broad coverage many Australians face significant financial barriers to accessing timely skin cancer diagnosis and treatment.
While Medicare provides bulk billing for general consultations, skin cancer checks and related procedures often require upfront payment, with only partial rebates available.
Patients are treated either by a GP or could be referred to a specialist.
Treatments include biopsies, surgical excision (predominantly), cautery and curettage, cryotherapy, or topical lotions. A small proportion of patients are treated in hospitals with wide excision, radiotherapy (for perineural invasion), or Mohs micrographic surgery. Some patients also require a re-excision for unclear margins.
Follow-up skin examinations generally occur bi-annually for up to 5 years, as per guidelines.

Financial obstacles in accessing these services disproportionately affect low-income individuals, pensioners, and those in rural areas, where access to specialist care may be limited.
A national survey by the Daffodil Centre revealed that older men, particularly in regional areas, are increasingly turning to their GPs for skin cancer management, highlighting the need for improved access to affordable specialist care.
A report published by the Australian Institute of Health and Welfare in 2020 said timely access to healthcare leads to better health outcomes. Cost and availability of specialists was recognised as contributing factors to delays. And delayed diagnosis can lead to advanced stages of skin cancer, reduced treatment options, and poorer health outcomes.
Early detection is paramount in the fight against skin cancer. The increasing number of skin cancer cases managed by GPs, coupled with the high cost of treatment, underscores the urgent need for greater access to preventative screenings and timely specialist care.
The Melanoma Institute Australia’s call for free melanoma screening for high-risk individuals emphasises the importance of proactive measures to catch skin cancers early.
When people can’t afford proper healthcare, it leaves space for skin clinic rip-offs, exploitation and the erosion of trust
The fear surrounding skin cancer has created a lucrative market, with some clinics resorting to unethical practices.
This masthead discovered that “fear-based” marketing tactics and the offering of unnecessary or overpriced procedures not only burden patients financially but also damage the trust between healthcare providers and the community.
Potential Solutions: A Multi-faceted Approach
-Expand Bulk Billing: Expanding Medicare coverage to include comprehensive skin cancer screenings, biopsies, and minor procedures would remove financial barriers and ensure equitable access to early detection for all Australians.
-Regulate the Skin Clinic Industry: Stricter regulations and transparent pricing are essential to combat over-servicing and exploitation in the skin clinic industry, protecting patients from unnecessary financial burdens and ensuring their safety.
–Public Awareness and Education: Comprehensive public awareness campaigns, targeted education programs, and readily available information about sun safety, early detection, and resources can empower individuals to take control of their skin health.
Invest in Research and Innovation: Continued investment in skin cancer research is vital for developing new prevention strategies, innovative diagnostic tools, and more effective treatment options.
Strengthen the Healthcare Workforce: Addressing the shortage of dermatologists and other skin cancer specialists, particularly in rural and remote areas, is essential for providing timely and quality care to all Australians.
Integrated Specialist Healthcare based in Sydney: A Beacon of Hope
What is integrated healthcare? The World Health Organization defines integrated healthcare as:
“…bringing together inputs, delivery, management and organisation of services related to diagnosis, treatment, care, rehabilitation, and health promotion. Integration is a means to improve services in relation to access, quality, user satisfaction and efficiency.”
Put simply, it’s about joining together and putting systems in place to ensure you receive the care you need, from where you need it, when you need it.

Professor Anand Deva is the Director of Cosmetic and Plastic Surgery at the Faculty of Medicine and Health Sciences, Macquarie University and co-director of the Surgical Infection Research Group. Professor Deva has received support and grants from NSW Health to develop the integrated health system model
They are using this approach to pioneer treatment for skin cancer and other diseases.
They offer comprehensive skin cancer treatment services, including:
- Skin assessments and examinations
- Biopsies (including punch and shave biopsies)
- Surgical excisions of skin cancers
- Non-surgical treatments (such as topical creams and photodynamic therapy)
- Mole mapping and monitoring
- Dermatoscopy (magnified examination of skin lesions)
- Cryotherapy (freezing of minor skin lesions)
The Integrated Specialist Healthcare team includes:
- Specialist General Practitioners with advanced training in skin cancer medicine
- Dermatologists (skin specialists)
- Plastic surgeons (for complex skin cancer reconstructions) ISHC’s skin cancer services focus on early detection, effective treatment, and minimization of scarring.
They also offer education on skin cancer prevention and sun protection.
This writer, (Editor of the Sydney Times, Aksel Ritenis) has come to the conclusion that initiatives like Integrated Specialist Healthcare, offering bulk-billed skin checks with immediate follow-up procedures and on-the-spot pathology, showcase effective solutions to improve access to timely and comprehensive skin cancer care.
Such models alleviate financial concerns and reduce wait times for diagnosis and treatment, improving patient outcomes.
“As a Pensioner and Medicare bulk bill patient the writer received Cryotherapy (freezing of minor skin lesions) on my head by Dr Martin Jaffe who gave me a visual examination and made an immediate assessment without any need for expensive pathology services or any time wasting referral to a Specialist. He then used the Cryotherapy method to remove skin lesions on my bald head. It was all very fast and efficient, and this is clearly the model that needs to be used to reduce the drag on resources and expedite treatment of skin cancer or potential melanomas.”
“The whole concept in a nutshell …is that Integrated healthcare for detecting melanoma refers to a comprehensive and coordinated approach to skin cancer care, where multiple healthcare professionals and services work together to provide seamless and patient-centred care.”

The above detailed approach aims to:
- Improve early detection and diagnosis of melanoma
- Enhance treatment outcomes
- Reduce fragmentation and duplication of services
- Foster collaboration and communication among healthcare providers
- Provide patient-centred care, considering individual needs and preferences
Integrated healthcare for melanoma detection may involve:
- Multidisciplinary teams: Dermatologists, general practitioners, surgeons, oncologists, and pathologists working together
- Coordinated care pathways: Streamlined referral processes and clear guidelines for diagnosis, treatment, and follow-up
- Shared electronic health records: Secure and accessible patient information for all involved healthcare providers
- Patient education and engagement: Empowering patients with knowledge and support throughout their care journey
- Continuous quality improvement: Regular review and refinement of care processes to ensure best practices and optimal outcomes By integrating healthcare services, patients receive more efficient, effective, and personalised care, leading to better detection and treatment of melanoma.
Conclusion: A Call to Action
-The skin cancer crisis in Australia demands immediate and decisive action from policymakers, healthcare providers, and the community at large.
-The human and economic costs of this silent epidemic are staggering, but through concerted efforts, we can turn the tide.
-By addressing financial barriers, regulating the industry, raising public awareness, and investing in research and healthcare infrastructure, Australia can make significant strides in reducing the burden of skin cancer and saving countless lives.